Gabapentin for Treatment of Carpal Tunnel Syndrome
My Doctor prescribed Gabapentin for the treatment of my Carpal Tunnel Syndrome Symptoms.
Is this a good treatment option for CTS?
Marilynn
Columbus, Ohio
Answers by Doctors at First Hand Medical
Gabapentin was developed and labeled with the FDA to be used with other medications to prevent and control seizures. It was never initially intend for the treatment of chronic syndromes like Carpal Tunnel. It is also labeled to be used to relieve nerve pain following shingles (a painful rash due to herpes zoster infection) in adults. Gabapentin is well-known among Neurologists as an anticonvulsant or antiepileptic drug.
Gabapentin is not a narcotic and is not a controlled substance. You might get confused about this because Gabapentin is often prescribed off-label as a painkiller and some have speculated that because it is not registered as a narcotic and is not a controlled substance, but acts like one, that:
“Gabapentin may be the most dangerous drug in America.”
https://www.dentistryiq.com/articles/2018/06/gabapentin-the-most-dangerous-drug-in-america.html
Gabapentin is an anticonvulsant and is approved by the FDA Label to prevent seizures in people with epilepsy. It also claims to be able to calm nerve pain and cause relaxation in the patient. This pharmaceutical has seen wider use recently in helping patients with addictions to scale back slowly from the withdrawal symptoms of quitting “cold turkey” from more harsh drug addictions in drug rehabilitation clinics.
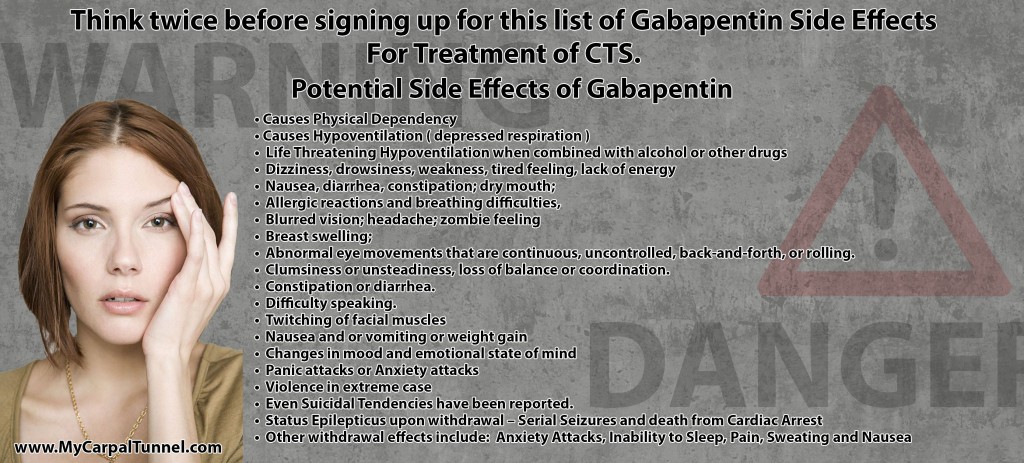
There are a multitude of potential side effects that can accompany the use of Gabapentin. These include:
What About Combining Medications with Gabapentin

Extreme care must be used by the patient not to combine other medications with Gabapentin due to the dangerous potential side effects. If someone uses Gabapentin and hydrocodone together, it can cause severe side effects like respiratory depression and even death. Since both are pain medications, some clinicians have been in the practice of prescribing both an opioid and Gabapentin at the same time.
Drinking alcohol and taking Gabapentin can cause extreme drowsiness or dizziness, and even respiratory depression and death. Patients are strongly advised not to drink alcohol or take opioid medication when taking Gabapentin. Other interactions include interactions with NSAIDs like naproxen, which is available in over-the-counter medications like Aleve. Any other medications a patient may be taking must be carefully evaluated for possible interactions with Gabapentin.
Gabapentin dosing must follow strict time requirements.
Care must be taken to assure that Gabapentin is taken at the prescribed times each day without missing the medication window. Taking the doses of this medication too far apart or too close together can cause complications.
It is also Dangerous to Stop Using Gabapentin all at once.
Not only does Gabapentin have many serious side effects, but withdrawing from the Medication can be even more dangerous if not monitored closely.
While this medication is not considered habit forming, Gabapentin causes physical dependence, which means if someone stops using it suddenly they may go through withdrawal. Withdrawal from gabapentin can be dangerous or life-threatening.
Severe withdrawal symptoms often occur when someone stops taking it suddenly. No one should stop taking gabapentin without speaking to their doctor and getting a specific prescribed protocol for slowly reducing exposure to the medication.
Sudden Withdrawal of Gabapentin can lead to serious withdrawal effects.
- Status Epilepticus = Serial Seizures and death from Cardiac Arrest
Other withdrawal effects include:
- Anxiety Attacks,
- Inability to Sleep,
- Pain,
- Sweating
- Nausea
Sudden withdrawal can cause a condition called Status Epilepticus. This condition is where the patient experiences serial seizures one after another creating a serious medical emergency that can result in sudden cardiac arrest and death. A patient must get to an emergency room immediately if this occurs.
Other withdrawal symptoms that can occur include anxiety, sleep problems, pain, sweating and nausea.
To avoid these symptoms, a physician will usually instruct patients reduce their gabapentin dosage gradually. It is possible to overdose on gabapentin as well, so following doctor’s instructions explicitly is important. Due to the ability of gabapentin to be used to treat certain pain conditions, people tend to wonder if it’s addictive. When taken as prescribed gabapentin isn’t considered habit-forming; however, people may misuse it recreationally. Gabapentin taken at high doses may cause euphoria or sedation. Because of how available gabapentin is and the fact that it’s not considered a controlled substance, it’s is often abused by those seeking to get “high” either with opioids or instead of opioids.
A patient should never take gabapentin without a prescription or outside of the realm of your doctor’s instructions.
If you’re struggling with gabapentin misuse, or someone you love may have substance use disorder, contact medical professionals in your area with expertise in dealing with substance abuse. https://www.therecoveryvillage.com/gabapentin-addiction/gabapentin-safe/#gref
Is Gabapentin Recommended to Treat Carpal Tunnel?
Given the Information Available on Gabapentin,
You might ask, “Would the Doctors at First Hand Medical recommend Gabapentin as a viable treatment option for Carpal Tunnel Syndrome?”
The suggestion of First Hand Medical would be:
It is difficult to imagine any circumstances where the use of Gabapentin would be recommended for the treatment of Carpal Tunnel Syndrome. There are just too many risks associated with starting treatment with this medication and also too many risks with ending treatment of this medication. There are much better options for treating Carpal Tunnel Syndrome than resorting to a drug with such a checkered history, complicated dosing and withdrawal instructions and overall risk factors.
Since Carpal Tunnel is a chronic disorder that comes back often throughout one’s life, it is the opinion of First Hand Medical that oral pain medication is a poor choice for treatment of this condition. https://www.mycarpaltunnel.com/oral-pain-medication-carpal-tunnel-treatment-reviewed-doctors.shtml

Oral pain medication options have little, if any, effect on mitigating the symptoms of this chronic hand disorder. The restriction in blood flow to the Carpal Tunnel caused by the pressure on the nerve which also imposes pressure on nearby blood vessels, minimizes the impact of oral pain medication on Carpal Tunnel Syndrome.

While pain medication can take the edge off of the worst symptoms of CTS temporarily for some people, it is our understanding that Gabapentin is not therapeutic in treating the cause of Carpal Tunnel Syndrome and we have seen no evidence to suggest that it is therapeutic in any way. It is our opinion that the risks and the potential discomfort and psychological effects that can result from using Gabapentin are too threatening to the patient to justify any of the minimal short-term benefits that it may seem to offer to a patient with Carpal Tunnel Syndrome.
Is Gabapentin an Opioid?
Patients often wonder, “is gabapentin an opioid?” Opioids are a class of drugs also known as narcotics that are tightly regulated by the US government.
This drug class includes habit-forming prescription painkillers, as well as heroin.
There are a few reasons people might incorrectly think gabapentin is an opioid.
First, gabapentin can be used as a pain reliever, and the primary use of opioids in a medical setting is to relieve pain.
Gabapentin can also lead to sedation, which is a major side effect of opioids.
When taken at high doses it is possible for some people to feel a sensation of being “high” from gabapentin, and again, this is an effect of opioids.
With both gabapentin and opioids is the potential for physical dependence.
Dependence isn’t the same as addiction.
Addiction is a chronic disease where a person is psychologically dependent on a substance.
It’s characterized by symptoms like compulsive drug use and drug-seeking behaviors.
Dependence, on the other hand, refers to a scenario where a person is physically, not psychologically, dependent on a medication or drug.
If someone is dependent on Gabapentin and stops taking it suddenly, they may go through withdrawal as describe above. Gabapentin withdrawal can be severe or deadly because it can trigger continuous seizures. People should only stop taking gabapentin on the advice of their doctor.
Physical withdrawal can occur with opioids as well, although the symptoms aren’t usually as severe as what can occur with gabapentin. Despite some of the similarities, gabapentin isn’t an opioid. It’s classified as an anticonvulsant, and there are some differences between this drug and opioids.
First, Gabapentin isn’t generally considered addictive psychologically. Opioids, on the other hand, are extremely addictive psychologically. Gabapentin doesn’t affect the central nervous system in the same way as opioids do, either. Gabapentin is believed to affect GABA levels but it does not bind to opioid receptors in the brain.
Opioids do bind to these opioid receptors, which is why they have the psychological effects. Gabapentin isn’t currently a controlled substance in the U.S., while opioids are a controlled substance in the United States of America.
Prescription opioids are carefully regulated and controlled in the U.S.A, while heroin is completely illegal with serious legal penalties for possession, trade or use.
Even though Gabapentin isn’t an opioid, there is scientific evidence showing that using these types of drugs together can raise the risk of an opioid-related death.
A recent study showed that people who combined opioids and gabapentin simultaneously had an increased chance of dying from opioids as compared to people who only took opioids.
This is particularly frightening because it’s not uncommon for gabapentin and opioids to be prescribed together to treat chronic pain.
Both Opioids and Gabapentin can suppress respiration, however, and that’s what can lead to a fatal overdose of either one or the other individually or when both are used together, the danger escalates dramatically. These medications should not be used together unless the patient is constantly monitored in a clinical setting such as an addiction recovery clinic. The danger of respiratory arrest and sudden death is too great when used together.
Gabapentin, opioids, and the risk of opioid-related death: A population-based nested case–control study
PLoS Med. 2017 Oct; 14(10): e1002396. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5626029/
In summary, Gabapentin isn’t technically an opioid. It does have many similarities to the Opioid class of Medication, including the potential to cause respiratory depression and the ability to lead to the development of physical dependence. Unlike Opioids, Gabapentin is not considered yet to create psychological dependency. It is a fine line in trying to separate Gabapentin from Opioids as a class of medication.
Gabapentin Off Label Use for Carpal Tunnel Syndrome Treatment Has Not be Approved by The FDA.
The fact that Gabapentin is being widely prescribed “Off-Label for Carpal Tunnel Syndrome Nerve Pain” is an interesting application. Gabapentin was originally developed, studied and submitted to the FDA for evaluation and approval as a treatment for epilepsy patients to prevent and minimize seizures. It has never been studied or evaluated by the FDA for the treatment of nerve pain from Carpal Tunnel Syndrome. This is not uncommon in the “practice of medicine” by Doctors. In fact, that may be why they call it “practicing medicine”. It is still not a perfect science. WebMD states that one in five prescriptions that are made by Doctors are “Off-Label”. So it is definitely not unusual. Still, treating nerve pain with a drug that has such a checked history, has so many potential side effects and has no documented therapeutic effect on improving Carpal Tunnel Syndrome, seems suspect to us, at best. The only targeted benefit is to reduce nerve pain – but at what risk to the patient.
https://www.webmd.com/a-to-z-guides/features/off-label-drug-use-what-you-need-to-know#1
Again, The Doctors at First Hand Medical strongly suggest that you should avoid the use of this oral pain medication that is being prescribed “Off-Label” for Carpal Tunnel Syndrome Treatment. It is just too dangerous to justify the prescription of Gabapentin for patient’s use “Off-Label” and unstudied, in our opinion.
First Hand Medical recommends all patients avoid all classes of Oral Medication for the treatment of Carpal Tunnel Syndrome.
Since Carpal Tunnel Syndrome is a chronic condition that comes back even after a Carpal Tunnel Surgical Procedure, First Hand Medical recommends a natural stretching protocol as the best first line treatment option to treat Carpal Tunnel Syndrome. Have hope, there is a much better Treatment option for patients with Carpal Tunnel Syndrome.